Bursitis Of The Feet Pain Therapy
Heel pain can also be caused due a condition called Bursitis which is constant irritation of the heel's natural cushion (bursa). This can lead to additional pain at the back of the heel when the ankle is moved and there may be swelling on both sides of the Achilles tendon. Useful treatments for Heel bursitis are anti-inflammatory medications such as aspirin and Ibuprofen gel/tablets. Cold ice-pack compresses can be useful in reducing any swelling. In conjunction to these treatments it is important to stabalise and protect the heel. Gel heel pads will help to let the inflamed bursa settle down, however in severe chronic cases sometimes the use of Cortisone injections may be indicated.
Causes
Certain medical conditions and medications suppress people's immune systems and make them more susceptible to septic bursitis. For example, people with cancer, HIV/AIDS, lupus, alcoholism, chronic obstructive pulmonary disease (COPD), and diabetes may be more likely to get septic bursitis. History of inflammation of the bursa. Patients who have had bursitis in the past have an increased chance of getting it again. There may be more than one reason why the retrocalcaneal bursa is inflamed. In these cases, treatment should address all of the causes.
Symptoms
Symptoms of bursitis include pain in the heel, especially with walking, running, or when the area is touched. The skin over the back of the heel may be red and warm, and the pain may be worse with attempted toe rise (standing on tippy-toes).
Diagnosis
Carrying out a diagnosis for bursitis is fairly straightforward. The doctor will examine the affected area and ask the patient some questions about his/her recent activities. If the patient has a high temperature the physician may take a small sample of fluid from a bursa near the affected body part. The sample will be tested for bacteria, and perhaps also crystals. If the patient does not get better after treatment the doctor may carry out further tests so that he/she can eliminate the possibility that the symptoms might not be due to something else. These may include an x-ray, to make sure no bones are broken or fractured. Blood tests, to check for rheumatoid arthritis. A CT scan or MRI scan to see if there is a torn tendon.
Non Surgical Treatment
In addition to R.I.C.E., there are a number of other treatments to reduce swelling and any associated pain or discomfort due to heel bursitis. Orthotics or change of footwear. Wearing an orthotic device such as a heel insert can encourage better mechanics in the foot and reduce irritation of the retrocalcaneal bursa. Some people do not need special orthotics but simply need to stop wearing shoes with rigid heel and ankle construction and instead wear more supportive, comfortable shoes. Shoes with an "Achilles notch," a groove in the collar at the back of the shoe to protect the Achilles tendon, can be particularly helpful. (Almost all running shoes are designed with an Achilles notch.) Stretching and physical therapy. Stretching the Achilles tendon often helps alleviate pain. Once the pain is resolved it is important for the patient to continue a regular stretching program. Regular stretching reduces the chance of recurrence.
Prevention
Do not run if you have pain. When you begin running again, avoid running fast uphill or downhill until the tendon is fully healed. Start exercising when caregivers say that it is OK. Slowly start exercise such as bicycling when caregivers say it is OK. When doing exercises that put pressure on the ankles, such as running or walking, exercise on flat, even surfaces. Avoid doing these exercises on very hard surfaces such as asphalt or concrete. Stretch before exercising. Always warm up your muscles and stretch gently before exercising. Do cool down exercises when you are finished. This will loosen your muscles and decrease stress on your heel. Wear heel protectors. Use soft foam or felt heel pads (wedges or cups) to help decrease pressure against your heel. Ask your caregiver which heel pads are the best for you. Wear well-fitting shoes. Buy running or exercise shoes that support and fit your feet well. Do not wear low-cut shoes. Talk to your caregiver or go to a special exercise footwear store to get well-fitting athletic shoes. Ask your caregiver if you should wear specially-made shoe inserts called orthotics (or-THOT-iks). Orthotics can line up your feet in your shoes to help you run, walk and exercise correctly.
Chiropractic Solution For Hammer Toes
 Overview
Overview
The smallest four toes of each foot have three bony segments connected by two joints. Hammertoe is a deformity in which one or more of the small toes develops a bend at the joint between the first and second segments. The tip of the toe turns downward, making it look like a hammer or claw. The second toe is the one most often affected. hammertoes may be more likely to occur when the second toe is longer than the first toe or when the arch of the foot is flat.
Causes
Hammertoes are more commonly seen in women than men, due to the shoe styles women frequently wear: shoes with tight toe boxes and high heels. Genetics plays a role in some cases of hammertoes, as does trauma, infection, arthritis, and certain neurological and muscle disorders. But most cases of contracted toes are associated with various biomechanical abnormalities of the feet, such as flat feet and feet with abnormally high arches. These biomechanical abnormalities cause the muscles and tendons to be used excessively or improperly, which deforms the toes over time.
 Symptoms
Symptoms
Common symptoms of hammertoes include pain or irritation of the affected toe when wearing shoes. corns and calluses (a buildup of skin) on the toe, between two toes, or on the ball of the foot. Corns are caused by constant friction against the shoe. They may be soft or hard, depending upon their location. Inflammation, redness, or a burning sensation. Contracture of the toe. In more severe cases of hammertoe, open sores may form.
Diagnosis
Although hammertoes are readily apparent, to arrive at a diagnosis the foot and ankle surgeon will obtain a thorough history Hammer toes of your symptoms and examine your foot. During the physical examination, the doctor may attempt to reproduce your symptoms by manipulating your foot and will study the contractures of the toes. In addition, the foot and ankle surgeon may take x-rays to determine the degree of the deformities and assess any changes that may have occurred.
Non Surgical Treatment
You should seek medical advice if you have a hammer toe. Here are some things you can do in the meantime. None of these things will cure the hammer toe, but they may relieve the pain and discomfort. Only wear shoes that are high and broad across the toes. There should be at least 1.5 cm of space between your longest toe and the tip of the shoe. Keep in mind that this could be either your big toe or your second toe. Don't wear heels higher than 5 cm. Wear the appropriate shoe for the activity you are doing. You can buy non-medicated hammer toe pads. They fit around the pointy top of the toe joint and help relieve painful pressure. Gently massaging the toe may help relieve pain. Put ice packs wrapped in cloth on the hammer toe to reduce painful swelling.
Surgical Treatment
The technique the surgeon applies during the surgery depends on how much flexibility the person's affected toes still retain. If some flexibility has still been preserved in their affected toes, the hammer toes might be corrected through making a small incision into the toe so the surgeon can manipulate the tendon that is forcing the person's toes into a curved position. If, however, the person's toes have become completely rigid, the surgeon might have to do more than re-aligning the person's tendons. Some pieces of bone may have to be removed so the person's toe has the ability to straighten out. If this is the case, some pins are attached onto the person's foot afterwards to fix their bones into place while the injured tissue heals.
Bilateral Hallux Valgus In Children
Overview
 The term bunion as it is popularly used describes a variety of deformities involving a painful prominence and swelling at the base of the big toe. Orthopaedists use additional terms to describe the different deformities. The condition in which the big toe deviates from the normal position toward the direction of the second toe is referred to as hallux valgus. The word bunion refers specifically to the prominence made of bone and at times an inflamed bursa. This bursa develops on the first metatarsal head at the base of the big toe because of this bony prominence. Although a bunion may develop without hallux valgus, for the purposes of this discussion, the term bunion will include both. Dorsal bunions, are a separate entity, in which the prominence appears on the top of the base of the toe-often the result of an arthritic joint.
The term bunion as it is popularly used describes a variety of deformities involving a painful prominence and swelling at the base of the big toe. Orthopaedists use additional terms to describe the different deformities. The condition in which the big toe deviates from the normal position toward the direction of the second toe is referred to as hallux valgus. The word bunion refers specifically to the prominence made of bone and at times an inflamed bursa. This bursa develops on the first metatarsal head at the base of the big toe because of this bony prominence. Although a bunion may develop without hallux valgus, for the purposes of this discussion, the term bunion will include both. Dorsal bunions, are a separate entity, in which the prominence appears on the top of the base of the toe-often the result of an arthritic joint.
Causes
By far the most common cause of bunions is the prolonged wearing of poorly fitting shoes, usually shoes with a narrow, pointed toe box that squeezes the toes into an unnatural position. Bunions also may be caused by arthritis or polio. Heredity often plays a role in bunion formation. But these causes account for only a small percentage of bunions. A study by the American Orthopaedic Foot and Ankle Society found that 88 percent of women in the U.S. wear shoes that are too small and 55 percent have bunions. Not surprisingly, bunions are nine times more common in women than men.
Symptoms
The dominant symptom of a bunion is a big bulging bump on the inside of the base of the big toe. Other symptoms include swelling, soreness and redness around the big toe joint, a tough callus at the bottom of the big toe and persistent or intermittent pain.
Diagnosis
Most patients are diagnosed to have bunions from clinical history and examination. However, in some cases, X-rays will be performed to determine the extent of damage to the joint. Furthermore, it will enable the treating doctor to decide on the best course of management of the patient.
Non Surgical Treatment
Treatment of hallux valgus nearly always starts with adapting shoe wear to fit the foot. In the early stages of hallux valgus, converting from a shoe with a pointed toe to a shoe with a wide forefoot (or toe box) may arrest the progression of the deformity. Since the pain that arises from the bunion is due to pressure from the shoe, treatment focuses on removing the pressure that the shoe exerts on the deformity. Wider shoes reduce the pressure on the bunion. Bunion pads may reduce pressure and rubbing from the shoe. There are also numerous devices, such as toe spacers, that attempt to splint the big toe and reverse the deforming forces. 
Surgical Treatment
There is no "standard" bunion, but rather a complex range of joint, bone, muscle, tendon and ligament abnormalities that can cause variation in each bunion's make-up. As a result, there are a broad variety of surgical techniques for dealing with bunions. Most surgical procedures start with a simple bunionectomy, which involves excision of swollen tissues and removal of the enlarged boney structure. While this may remove the troublesome tissues, however, it may not correct other issues associated with the bunion. The surgeon may also need to tighten or loosen the muscles, tendons and ligaments around the MTP joint. Realign the bone by cutting it and shifting its position (a technique called osteotomy), realigning muscles, tendons and ligaments accordingly. Use screws, wires or plates to hold the joint surfaces together until they heal. Reconstruct a badly damaged joint or replace it with an artificial implant.
Overpronation Pain And Discomfort
Pronation describes the natural process of the inward rolling of your foot when the outer edge of your heel strikes the ground and your foot flattens out. Excess pronation, known as flat foot, can result in flattened arches and overstretched foot muscles. Advanced conditions may affect your hips, knees, ankle, back and foot functioning. Use natural techniques to stretch and strengthen your muscles in order to help pronation.

Causes
There are many biomechanical issues that can contribute to excessive pronation, including weak foot intrinsic muscles, limited ankle dorsiflexion mobility and calf flexibility, weak ankle invertor muscles (e.g. posterior tibialis), weak forefoot evertor muscles (peroneus longus), poor hip strength and control, Anterior pelvic tilting, heel InversionIn a person who overpronates, the heel bone goes into an everted position meaning that it turns out away from the midline of the body. The opposite motion of eversion is inversion. Inversion is a motion that needs to be controlled to prevent the foot from excessively pronating.
Symptoms
Because overpronation affects the entire lower leg, many injuries and conditions may develop and eventually cause problems not only in the leg and foot, but also the knee, hips and lower back. Pain often begins in the arch of the foot or the ankle. Blisters may develop on the instep, or on the inside edge of the heels. As overpronation continues and problems develop, pain will be felt elsewhere, depending on the injury.
Diagnosis
When sitting, an over-pronating foot appears quite normal, i.e. showing a normal arch with room under the underside of the foot. The moment you get up and put weight on your feet the situation changes: the arches lower and the ankle slightly turns inwards. When you walk or run more weight is placed on the feet compared to standing and over-pronation will become more evident. When walking barefoot on tiles or timber floors over-pronation is more visible, compared to walking on carpet or grass.

Non Surgical Treatment
Overpronation is a condition in which the foot rolls excessively down and inward. The arch may elongate and collapse (or ?fall?) and the heel will lean inward. Overpronation should not be confused with pronation. Pronation is a normal motion of the foot during weight bearing and allows the foot to absorb shock as it contacts the ground.
Prevention
Custom-made orthotics will reduce the twisting of the leg muscles as they enter the foot, by maintaining a normal alignment of the bones and joints of the foot. If the bones and joints are aligned properly, by reducing the pronation, the muscles can run straight to their attachments in the foot, without twisting to get to these bones. This action of custom-made orthotics will reduce Achilles Tendonitis shin splints; ankle, knee, hip, and lower back pain; and leg cramps. This action will also allow the leg muscles to work more efficiently, thus allowing you to walk and run with less effort.
Therapy For Calcaneal Apophysitis
Sever?s disease is a common cause of heel pain in children especially in the young and physically active. Severs disease is a painful bone disorder that results from inflammation (swelling) of the growth plate in the heel. A growth plate, also called an epiphyseal plate, is an area at the end of a developing bone where cartilage cells change over time into bone cells. As this occurs, the growth plates expand and unite. It is very important that damage to the growth plate is avoided.
Causes
Sever's disease is caused by repetitive tension and/or pressure on the growth center of the heel. Running and jumping place a large amount of pressure on the heels and can cause pain. Children with Sever's may limp or have an altered gait due to the pain. Risk factors for Sever's include tight calf muscles, weak ankle muscles, and alignment abnormalities at the foot and ankle. Sever's can also result from wearing shoes without sufficient heel padding or arch support.
Symptoms
If your child is suffering from this disease they will be experiencing pain and tenderness in the back of their foot. This soreness can also extend to the sides of the feet. Other sure signs of this disorder include swelling and sensitivity to touch. Because of the amount of discomfort, your child may find it difficult to walk or run. Pay attention to the way your child is walking. If you notice unusual posture or abnormal gait they may be avoiding placing pressure on the heel. These symptoms typically become apparent during activity and exercise or directly following it. If your child is indicating pain in their heel, schedule an appointment with us today.
Diagnosis
Sever?s disease can be diagnosed based on your history and symptoms. Clinically, your physiotherapist will perform a "squeeze test" and some other tests to confirm the diagnosis. Some children suffer Sever?s disease even though they do less exercise than other. This indicates that it is not just training volume that is at play. Foot and leg biomechanics are a predisposing factor. The main factors thought to predispose a child to Sever?s disease include decrease ankle dorsiflexion, abnormal hind foot motion eg overpronation or supination, tight calf muscles, excessive weight-bearing activities eg running.
Non Surgical Treatment
The following are different treatment options. Rest and modify activity. Limit running and high-impact activity to rest the heel and lessen the pain. Choose one running or jumping sport to play at a time. Substitute low-impact cross-training activities to maintain cardiovascular fitness. This can include biking, swimming, using a stair-climber or elliptical machine, rowing, or inline skating. Reduce inflammation. Ice for at least 20 minutes after activity or when pain increases. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also help. Stretch the calf. Increase calf flexibility by doing calf stretches for 30 to 45 seconds several times per day. Protect the heel. The shoe may need to be modified to provide the proper heel lift or arch support. Select a shoe with good arch support and heel lift if possible. Try heel lifts or heel cups in sports shoes, especially cleats. Try arch support in cleats if flat feet contribute to the problem.
Acute Achilles Tendon Rupture Surgery Cost
Overview
 The Achilles tendon is the largest tendon in the body; connecting the calf muscles to the heel. An Achilles tendon rupture prevents the tendon from performing its function of pulling the foot and ankle downward during walking, running and jumping. Most ruptures occur about four to six inches above the heel, but the tendon can also tear where it meets the heel bone.
The Achilles tendon is the largest tendon in the body; connecting the calf muscles to the heel. An Achilles tendon rupture prevents the tendon from performing its function of pulling the foot and ankle downward during walking, running and jumping. Most ruptures occur about four to six inches above the heel, but the tendon can also tear where it meets the heel bone.
Causes
As with any muscle or tendon in the body, the Achilles tendon can be torn if there is a high force or stress on it. This can happen with activities which involve a forceful push off with the foot, for example, in football, running, basketball, diving, and tennis. The push off movement uses a strong contraction of the calf muscles which can stress the Achilles tendon too much. The Achilles tendon can also be damaged by injuries such as falls, if the foot is suddenly forced into an upward-pointing position, this movement stretches the tendon. Another possible injury is a deep cut at the back of the ankle, which might go into the tendon. Sometimes the Achilles tendon is weak, making it more prone to rupture. Factors that weaken the Achilles tendon are as follows. Corticosteroid medication (such as prednisolone) - mainly if it is used as long-term treatment rather than a short course. Corticosteroid injection near the Achilles tendon. Certain rare medical conditions, such as Cushing's syndrome, where the body makes too much of its own corticosteroid hormones. Increasing age. Tendonitis (inflammation) of the Achilles tendon. Other medical conditions which can make the tendon more prone to rupture; for example, rheumatoid arthritis, gout and systemic lupus erythematosus (SLE), lupus. Certain antibiotic medicines may slightly increase the risk of having an Achilles tendon rupture. These are the quinolone antibiotics such as ciprofloxacin and ofloxacin. The risk of having an Achilles tendon rupture with these antibiotics is actually very low, and mainly applies if you are also taking corticosteroid medication or are over the age of about 60.
Symptoms
Often the person feels a whip-like blow that is followed by weakness in the affected leg - usually he or she is not able to walk afterwards. At place where the tendon ruptured, a significant dent is palpable. Often the experienced physician can diagnose a ruptured Achilles tendon by way of clinical examination and special function tests. Imaging techniques, such as ultrasound and magnetic resonance imaging (MRI) allow for a more precise diagnosis.
Diagnosis
An Achilles' tendon injury can be diagnosed by applying the Thompson Test (or Calf Squeeze Test) this is where the person who has suffered the injury lies on their front with their legs bent. Whoever is performing the test, usually a doctor, will then squeeze the calf muscle. If the tendon has not ruptured then the foot should point briefly away from the leg.
Non Surgical Treatment
The treatments of Achilles tendonitis include resting the painful Achilles tendon will allow the inflammation to subside and allow for healing. A period of rest after the onset of symptoms is important in controlling Achilles tendonitis. In patients who have more significant symptoms, a period of immobilization can help. Either a removable walking boot or a cast can allow the inflamed tendon to cool down quickly. A heel wedge can be inserted into the shoe to minimize the stress on the Achilles tendon. These can be placed in both athletic and work shoes. Applying ice to the area of inflammation can help stimulate blood flow to the area and relieve the pain associated with inflammation. Apply ice several times a day, including after exercise. The pain and swelling most commonly associated with Achilles tendonitis can be improved with non-steroidal, anti-inflammatory medications (NSAIDs) which include Celebrex?, Advil?, Motrin?, Naprosyn?. Be sure to consult your physician before starting any medications. Physical therapists can help formulate a stretching and rehabilitation program to improve flexibility of the Achilles tendon. Cortisone injections should not be used for Achilles tendonitis. Studies have shown an increased incidence of Achilles tendon rupture after cortisone injections. 
Surgical Treatment
A completely ruptured Achilles tendon requires surgery and up to 12 weeks in a cast. Partial tears are sometimes are treated with surgery following by a cast. Because the tendon shortens as it heals, a heel lift is used for 6 months or more after the cast comes off. Physical therapy to regain flexibility and then strength are begun as soon as the cast is off.
Surgery For Flat Feet In Adults
Overview
The posterior tibialis muscle originates on the bones of the leg (tibia and fibula). This muscle then passes behind the medial (inside) aspect of the ankle and attaches to the medial midfoot as the posterior tibial tendon. The posterior tibial tendon serves to invert (roll inward) the foot and maintain the arch of the foot. This tendon plays a central role in maintaining the normal alignment of the foot and also in enabling normal gait (walking). In addition to tendons running across the ankle and foot joints, a number of ligaments span and stabilize these joints. The ligaments at the medial ankle can become stretched and contribute to the progressive flattening of the arch. Several muscles and tendons around the ankle and foot act to counter-balance the action of the posterior tibial tendon. Under normal circumstances, the result is a balanced ankle and foot with normal motion. When the posterior tibial tendon fails, the other muscles and tendons become relatively over-powering. These muscles then contribute to the progressive deformity seen with this disorder. 
Causes
Flat feet causes greater pressure on the posterior tibial tendon than normal. As the person with flat feet ages, the muscles, tendons and ligaments weaken. Blood supplies diminish as arteries narrow. These conditions are magnified for obese patients because of their increased weight and atherosclerosis. Finally, the tendon gives out or tears. Most of the time, this is a slow process. Once the posterior tibial tendon and ligaments stretch, body weight causes the bones of the arch to move out of position. The foot rotates inward (pronation), the heel bone is tilted to the inside, and the arch appears collapsed. In some cases, the deformity progresses until the foot dislocates outward from the ankle joint.
Symptoms
Not everyone with adult flatfoot has problems with pain. Those who do usually experience it around the ankle or in the heel. The pain is usually worse with activity, like walking or standing for extended periods. Sometimes, if the condition develops from arthritis in the foot, bony spurs along the top and side of the foot develop and make wearing shoes more painful. Diabetic patients need to watch for swelling or large lumps in the feet, as they may not notice any pain. They are also at higher risk for developing significant deformities from their flatfoot.
Diagnosis
There are four stages of adult-acquired flatfoot deformity (AAFD). The severity of the deformity determines your stage. For example, Stage I means there is a flatfoot position but without deformity. Pain and swelling from tendinitis is common in this stage. Stage II there is a change in the foot alignment. This means a deformity is starting to develop. The physician can still move the bones back into place manually (passively). Stage III adult-acquired flatfoot deformity (AAFD) tells us there is a fixed deformity. This means the ankle is stiff or rigid and doesn???t move beyond a neutral (midline) position. Stage IV is characterized by deformity in the foot and the ankle. The deformity may be flexible or fixed. The joints often show signs of degenerative joint disease (arthritis).
Non surgical Treatment
Non-surgical treatment includes rest and reducing your activity until the pain improves. Orthotics or bracing help support the tendon to reduce its pull along the arch, thus reducing pain. In moderate to severe cases, a below knee cast or walking boot may be needed to allow the tendon to rest completely and heal. Physical therapy is an integral part of the non-surgical treatment regimen to reduce inflammation and pain. Anti-inflammatory medication is often used as well. Many times evaluation of your current shoes is necessary to ensure you are wearing appropriate shoe gear to prevent re-injury. 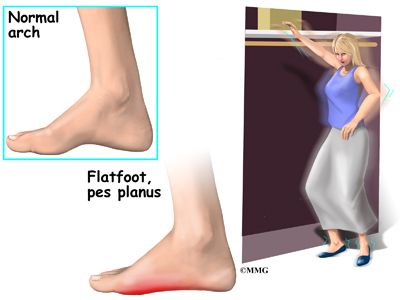
Surgical Treatment
Flatfoot reconstruction (osteotomy). This is often recommended for flexible flatfoot condition. Flatfoot reconstruction involves cutting and shifting the heel bone into a more neutral position, transferring the tendon used to flex the lesser toes (all but the big toe) to strengthen the posterior tibial tendon, and lengthening the calf muscle. Fusion (also known as triple arthrodesis). Fusion involves fusing, or making stiff, three joints in the back of the foot the subtalar, talonavicular, and calcaneocuboid joints, to realign the foot and give it a more natural shape. Pins or screws hold the area in place until it heals. Fusion is often recommended for a rigid flatfoot deformity or evidence of arthritis. Both of these surgeries can provide excellent pain relief and correction.