Guidelines On How To Combat Pes Planus
Overview
Most people (approx. 60-70% of the population) suffer from excessive pronation due to flat feet when walking, running and standing. Though the foot may appear normal when sitting down, with a clear arch present under the foot, over-pronation becomes noticeable when we stand or walk as a result of weight bearing. The arches collapse with every step we take, and the ankles roll inwards. This is called overpronation, a biomechanical imbalance that can lead to many painful foot conditions such as heel pain, plantar fasciitis, heel spurs, tendonitis, and can even affect other parts of your body such as the knees and lower back.
Causes
Over-pronation is a common biomechanical problem that occurs when the arches collapse while walking or standing. This condition hampers our natural walking pattern, causing an imbalance, and leading to wear and tear in other parts of the body with every step we take. Whether you suffer from over-pronation like most of the population, or you have a true flat foot, in both cases your poor walking pattern may contribute to a range of different complaints. As we age, poor aligment of the feet causes very common conditions such as heel pain or knee pain. Over-pronation has different causes. Obesity, pregnancy, age or repetitive pounding on a hard surface can weaken the arch, leading to over-pronation. Over-pronation is also very common with athletes, especially runners, who most of them nowadays use orthotics inside their shoes.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
It is important for people with foot pain to know if they have flat feet. The following tests can help you determine your arch type. When you get out of a swimming pool, look at your footprint on the concrete. The front of the foot will be joined to the heel by a strip. If your foot is flat, then the strip is the same width as the front of the foot, creating a footprint that looks like a stretched out pancake. With a normal arch, the strip is about half the width of the front of the foot. If you have a high arch, only a thin strip connects the front of the foot with the heel. Put your shoes on a flat table and view them at eye level from behind. See if the sole is worn evenly. A flat foot will cause more wear on the inside of the sole, especially in the heel area. The shoe will easily rock side to side. A flat foot will also cause the upper part of the shoe to lean inward over the sole. Both shoes should wear about the same way. If you have pain in one foot, you should make sure you don't have a fallen arch on that side. There are two good tests you can perform at home to detect this problem. Place your fingertips on a wall that you are directly facing and stand on your tiptoes on one foot. If you can't do it, a fallen arch may be the culprit. Stand with your feet parallel. Have someone stand in back of you and look at your feet from behind. You can also do it yourself if you stand with your back to a mirror. Normally, only the pinky toe is visible from behind. If one foot is flatter than the other, the 4th and sometimes the 3rd toe on that foot can also be seen.
pes planus exercises
Non Surgical Treatment
Treatment in adults generally consists of wearing spacious, comfortable shoes with good arch support. Your doctor may recommend padding for the heel (heel cup) or orthotic shoe devices, which are molded pieces of rubber, leather, metal, plastic, or other synthetic material that are inserted into a shoe. They balance the foot in a neutral position and cushion the foot from excessive pounding. For children, treatment using corrective shoes or inserts is rarely needed, as the arch usually develops normally by age 5.
Surgery is rarely needed.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
Prevention
Orthotic inserts, either prescribed or bought over the counter, can help keep the arches fixed into position, but always wear them as although they support, they don?t strengthen, which is why some experts reccomend avoiding them. Gait analysis at a run specialist can help to diagnose overpronation and flat feet. Most brands produce shoes that will give support and help to limit the negative effects of a poor gait on the rest of the body. Barefoot exercises, such as standing on a towel and making fists with the toes, can help to strengthen the arches. Start easy and build up the reps to avoid cramping. Short barefoot running sessions can help take pressure off the arches by using the natural elasticity of the foot?s tendons to take impact and build strength to help prevent flat feet. These should be done on grass for only a few minutes at a time.
Most people (approx. 60-70% of the population) suffer from excessive pronation due to flat feet when walking, running and standing. Though the foot may appear normal when sitting down, with a clear arch present under the foot, over-pronation becomes noticeable when we stand or walk as a result of weight bearing. The arches collapse with every step we take, and the ankles roll inwards. This is called overpronation, a biomechanical imbalance that can lead to many painful foot conditions such as heel pain, plantar fasciitis, heel spurs, tendonitis, and can even affect other parts of your body such as the knees and lower back.
Causes
Over-pronation is a common biomechanical problem that occurs when the arches collapse while walking or standing. This condition hampers our natural walking pattern, causing an imbalance, and leading to wear and tear in other parts of the body with every step we take. Whether you suffer from over-pronation like most of the population, or you have a true flat foot, in both cases your poor walking pattern may contribute to a range of different complaints. As we age, poor aligment of the feet causes very common conditions such as heel pain or knee pain. Over-pronation has different causes. Obesity, pregnancy, age or repetitive pounding on a hard surface can weaken the arch, leading to over-pronation. Over-pronation is also very common with athletes, especially runners, who most of them nowadays use orthotics inside their shoes.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
It is important for people with foot pain to know if they have flat feet. The following tests can help you determine your arch type. When you get out of a swimming pool, look at your footprint on the concrete. The front of the foot will be joined to the heel by a strip. If your foot is flat, then the strip is the same width as the front of the foot, creating a footprint that looks like a stretched out pancake. With a normal arch, the strip is about half the width of the front of the foot. If you have a high arch, only a thin strip connects the front of the foot with the heel. Put your shoes on a flat table and view them at eye level from behind. See if the sole is worn evenly. A flat foot will cause more wear on the inside of the sole, especially in the heel area. The shoe will easily rock side to side. A flat foot will also cause the upper part of the shoe to lean inward over the sole. Both shoes should wear about the same way. If you have pain in one foot, you should make sure you don't have a fallen arch on that side. There are two good tests you can perform at home to detect this problem. Place your fingertips on a wall that you are directly facing and stand on your tiptoes on one foot. If you can't do it, a fallen arch may be the culprit. Stand with your feet parallel. Have someone stand in back of you and look at your feet from behind. You can also do it yourself if you stand with your back to a mirror. Normally, only the pinky toe is visible from behind. If one foot is flatter than the other, the 4th and sometimes the 3rd toe on that foot can also be seen.
pes planus exercises
Non Surgical Treatment
Treatment in adults generally consists of wearing spacious, comfortable shoes with good arch support. Your doctor may recommend padding for the heel (heel cup) or orthotic shoe devices, which are molded pieces of rubber, leather, metal, plastic, or other synthetic material that are inserted into a shoe. They balance the foot in a neutral position and cushion the foot from excessive pounding. For children, treatment using corrective shoes or inserts is rarely needed, as the arch usually develops normally by age 5.
Surgery is rarely needed.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
Prevention
Orthotic inserts, either prescribed or bought over the counter, can help keep the arches fixed into position, but always wear them as although they support, they don?t strengthen, which is why some experts reccomend avoiding them. Gait analysis at a run specialist can help to diagnose overpronation and flat feet. Most brands produce shoes that will give support and help to limit the negative effects of a poor gait on the rest of the body. Barefoot exercises, such as standing on a towel and making fists with the toes, can help to strengthen the arches. Start easy and build up the reps to avoid cramping. Short barefoot running sessions can help take pressure off the arches by using the natural elasticity of the foot?s tendons to take impact and build strength to help prevent flat feet. These should be done on grass for only a few minutes at a time.
Do You Understand Heel Pains?
Overview

Your foot is made up of 26 bones, 33 joints, and more than 100 tendons. The heel is the largest bone in your foot. If you overuse or injure your heel, you may experience heel pain. This can range from mild to disabling. In many cases, if you have heel pain, you will need a doctor to diagnose the cause.
Causes
There are two different categories of heel pain. The first is caused by over-use repetitive stress which refers to a soreness resulting from too much impact on a specific area of the foot. This condition, often referred to as "heel pain syndrome," can be caused by shoes with heels that are too low, a thinned out fat pad in the heel area, or from a sudden increase in activity. Plantar fasciitis, a very common diagnosis of heel pain, is usually caused from a biomechancial problem, such as over-pronation (flat feet). The plantar fascia is a broad band of fibrous tissue that runs along the bottom surface of the foot, from the heel through the midfoot and into the forefoot. Over-pronation can cause the plantar fascia to be excessively stretched and inflamed, resulting in pain in the heel and arch areas of the foot. Often the pain will be most intense first thing in the morning or after a prolonged period of rest. The pain will gradually subside as the day progresses.
Symptoms
Depending on the specific form of heel pain, symptoms may vary. Pain stemming from plantar fasciitis or heel spurs is particularly acute following periods of rest, whether it is after getting out of bed in the morning, or getting up after a long period of sitting. In many cases, pain subsides during activity as injured tissue adjusts to damage, but can return again with prolonged activity or when excessive pressure is applied to the affected area. Extended periods of activity and/or strain of the foot can increase pain and inflammation in the foot. In addition to pain, heel conditions can also generate swelling, bruising, and redness. The foot may also be hot to the touch, experience tingling, or numbness depending on the condition.
Diagnosis
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Using our state-of-the-art equipment, Dr. Weinert is able to provide a full work up for the heel, including gait analysis. Digital imagining gives him and the patient a full view of the foot and injury to help formulate the best treatment plan possible. There are numerous treatment options available to help with heel pain and plantar fasciitis. Anti-inflammatory medications. Digital custom orthotics. Physical therapy. Diagnostic and ultrasonic guided injection therapy. No one should ever resign to living with foot pain.
Surgical Treatment
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
heel spur surgery
Prevention

Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain.

Your foot is made up of 26 bones, 33 joints, and more than 100 tendons. The heel is the largest bone in your foot. If you overuse or injure your heel, you may experience heel pain. This can range from mild to disabling. In many cases, if you have heel pain, you will need a doctor to diagnose the cause.
Causes
There are two different categories of heel pain. The first is caused by over-use repetitive stress which refers to a soreness resulting from too much impact on a specific area of the foot. This condition, often referred to as "heel pain syndrome," can be caused by shoes with heels that are too low, a thinned out fat pad in the heel area, or from a sudden increase in activity. Plantar fasciitis, a very common diagnosis of heel pain, is usually caused from a biomechancial problem, such as over-pronation (flat feet). The plantar fascia is a broad band of fibrous tissue that runs along the bottom surface of the foot, from the heel through the midfoot and into the forefoot. Over-pronation can cause the plantar fascia to be excessively stretched and inflamed, resulting in pain in the heel and arch areas of the foot. Often the pain will be most intense first thing in the morning or after a prolonged period of rest. The pain will gradually subside as the day progresses.
Symptoms
Depending on the specific form of heel pain, symptoms may vary. Pain stemming from plantar fasciitis or heel spurs is particularly acute following periods of rest, whether it is after getting out of bed in the morning, or getting up after a long period of sitting. In many cases, pain subsides during activity as injured tissue adjusts to damage, but can return again with prolonged activity or when excessive pressure is applied to the affected area. Extended periods of activity and/or strain of the foot can increase pain and inflammation in the foot. In addition to pain, heel conditions can also generate swelling, bruising, and redness. The foot may also be hot to the touch, experience tingling, or numbness depending on the condition.
Diagnosis
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Using our state-of-the-art equipment, Dr. Weinert is able to provide a full work up for the heel, including gait analysis. Digital imagining gives him and the patient a full view of the foot and injury to help formulate the best treatment plan possible. There are numerous treatment options available to help with heel pain and plantar fasciitis. Anti-inflammatory medications. Digital custom orthotics. Physical therapy. Diagnostic and ultrasonic guided injection therapy. No one should ever resign to living with foot pain.
Surgical Treatment
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
heel spur surgery
Prevention

Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain.
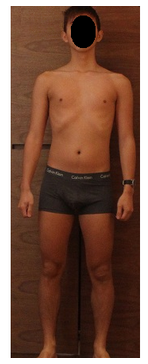
Treatment For Leg Length Discrepancy After Hip Replacement
Overview
The majority of people in the world actually have some degree of leg length discrepancy, up to 2cm. One study found that only around 1/4 of people have legs of equal lengths. LLD of greater than 2cm is relatively rare, however, and the greater the discrepancy, the greater the chances of having a clinical problem down the road. A limp generally begins when LLD exceeds 2cm and becomes extremely noticeable above 3cm. When patients with LLD develop an abnormal gait, one of the debilitating clinical features can be fatigue because of the relatively high amount of energy needed to walk in the new, inefficient way. Poliomyelitis, or polio, as it is more commonly known, used to account for around 1/3 of all cases of LLD, but due to the effectiveness of polio vaccines, it now represents a negligible cause of the condition. Functional LLD, described above, usually involves treatment focused on the hip, pelvis, and/or lower back, rather than the leg. If you have been diagnosed with functional LLD or pelvic obliquity, please ask your orthopaedic surgeon for more information about treatment of these conditions.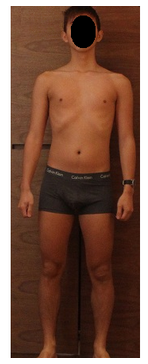
Causes
Leg discrepancy can develop from a medical issue in any portion of the femur or tibia. One leg may lengthen, but leg shortening is much more common. Factors that can cause leg length discrepancy include inherited growth deficiencies. Infections. A bone infection can cause delayed growth in the affected limb. Injury. If your child breaks a leg, it may be shorter once it heals. This is most likely to happen if the fracture or break was complicated, an open fracture, or an injury that affected the growth plate near the end of the bone. Alternatively, a break can cause bones to grow faster after healing, making a leg longer. Tumors. Legg-Calve-Perthes disease. This is a condition that affects the ball (femoral head) of the hip joint. The femoral head may be friable and damage easily, sometimes leading to shortening of the thigh bone. Hemihypertrophy. In children with this condition, one side of the body grows more quickly than the other. Vascular malformations. These are abnormal clusters of veins and arteries that can form close to the bone and stimulate growth. Juvenile arthritis. Inflammation from arthritis can stimulate growth in the affected leg and cause discrepancy.
Symptoms
The effects vary from patient to patient, depending on the cause of the discrepancy and the magnitude of the difference. Differences of 3 1/2 to 4 percent of the total length of the lower extremity (4 cm or 1 2/3 inches in an average adult), including the thigh, lower leg and foot, may cause noticeable abnormalities while walking and require more effort to walk. Differences between the lengths of the upper extremities cause few problems unless the difference is so great that it becomes difficult to hold objects or perform chores with both hands. You and your physician can decide what is right for you after discussing the causes, treatment options and risks and benefits of limb lengthening, including no treatment at all. Although an LLD may be detected on a screening examination for curvature of the spine (scoliosis), LLD does not cause scoliosis. There is controversy about the effect of LLD on the spine. Some studies indicate that people with an LLD have a greater incidence of low back pain and an increased susceptibility to injuries, but other studies refute this relationship.
Diagnosis
The only way to decipher between anatomical and functional leg length inequalities (you can have both) is by a physical measurement and series of biomechanical tests. It is actually a simple process and gets to the true cause of some runner?s chronic foot, knee, hip and back pain. After the muscles are tested and the legs are measured it may be necessary to get a special X-ray that measures both of your thighs (Femurs) and legs (Tibias). The X-ray is read by a medical radiologist who provides a report of the actual difference down to the micrometer leaving zero room for error. Once the difference in leg length is known, the solution becomes clear.
Non Surgical Treatment
Heel lifts and sole lifts are simple ways Pedorthists can compensate for leg length deficiencies. These small modifications can make a tremendous difference to a person?s comfort, balance and mobility. Although people do not always know if they have LLD if you have any of the symptoms I have mentioned you should consult a Pedorthist as treating your condition early will reduce the development of serious problems later on.

heelsncleavage
Surgical Treatment
The bone is lengthened by surgically applying an external fixation device to the leg. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins, or both. A small crack is made in the bone and the frame creates tension when the patient or family member turns its dial. This is done several times each day. The lengthening process begins approximately five to 10 days after surgery. The bone may lengthen 1 millimeter per day, or approximately 1 inch per month. Lengthening may be slower in a bone that was previously injured. It may also be slower if the leg was operated on before. Bones in patients with potential blood vessel abnormalities, such as cigarette smokers, may also need to be lengthened more slowly. The external fixator is worn until the bone is strong enough to support the patient safely. This usually takes about three months for each inch. Factors such as age, health, smoking and participation in rehabilitation can affect the amount of time needed.
The majority of people in the world actually have some degree of leg length discrepancy, up to 2cm. One study found that only around 1/4 of people have legs of equal lengths. LLD of greater than 2cm is relatively rare, however, and the greater the discrepancy, the greater the chances of having a clinical problem down the road. A limp generally begins when LLD exceeds 2cm and becomes extremely noticeable above 3cm. When patients with LLD develop an abnormal gait, one of the debilitating clinical features can be fatigue because of the relatively high amount of energy needed to walk in the new, inefficient way. Poliomyelitis, or polio, as it is more commonly known, used to account for around 1/3 of all cases of LLD, but due to the effectiveness of polio vaccines, it now represents a negligible cause of the condition. Functional LLD, described above, usually involves treatment focused on the hip, pelvis, and/or lower back, rather than the leg. If you have been diagnosed with functional LLD or pelvic obliquity, please ask your orthopaedic surgeon for more information about treatment of these conditions.
Causes
Leg discrepancy can develop from a medical issue in any portion of the femur or tibia. One leg may lengthen, but leg shortening is much more common. Factors that can cause leg length discrepancy include inherited growth deficiencies. Infections. A bone infection can cause delayed growth in the affected limb. Injury. If your child breaks a leg, it may be shorter once it heals. This is most likely to happen if the fracture or break was complicated, an open fracture, or an injury that affected the growth plate near the end of the bone. Alternatively, a break can cause bones to grow faster after healing, making a leg longer. Tumors. Legg-Calve-Perthes disease. This is a condition that affects the ball (femoral head) of the hip joint. The femoral head may be friable and damage easily, sometimes leading to shortening of the thigh bone. Hemihypertrophy. In children with this condition, one side of the body grows more quickly than the other. Vascular malformations. These are abnormal clusters of veins and arteries that can form close to the bone and stimulate growth. Juvenile arthritis. Inflammation from arthritis can stimulate growth in the affected leg and cause discrepancy.
Symptoms
The effects vary from patient to patient, depending on the cause of the discrepancy and the magnitude of the difference. Differences of 3 1/2 to 4 percent of the total length of the lower extremity (4 cm or 1 2/3 inches in an average adult), including the thigh, lower leg and foot, may cause noticeable abnormalities while walking and require more effort to walk. Differences between the lengths of the upper extremities cause few problems unless the difference is so great that it becomes difficult to hold objects or perform chores with both hands. You and your physician can decide what is right for you after discussing the causes, treatment options and risks and benefits of limb lengthening, including no treatment at all. Although an LLD may be detected on a screening examination for curvature of the spine (scoliosis), LLD does not cause scoliosis. There is controversy about the effect of LLD on the spine. Some studies indicate that people with an LLD have a greater incidence of low back pain and an increased susceptibility to injuries, but other studies refute this relationship.
Diagnosis
The only way to decipher between anatomical and functional leg length inequalities (you can have both) is by a physical measurement and series of biomechanical tests. It is actually a simple process and gets to the true cause of some runner?s chronic foot, knee, hip and back pain. After the muscles are tested and the legs are measured it may be necessary to get a special X-ray that measures both of your thighs (Femurs) and legs (Tibias). The X-ray is read by a medical radiologist who provides a report of the actual difference down to the micrometer leaving zero room for error. Once the difference in leg length is known, the solution becomes clear.
Non Surgical Treatment
Heel lifts and sole lifts are simple ways Pedorthists can compensate for leg length deficiencies. These small modifications can make a tremendous difference to a person?s comfort, balance and mobility. Although people do not always know if they have LLD if you have any of the symptoms I have mentioned you should consult a Pedorthist as treating your condition early will reduce the development of serious problems later on.

heelsncleavage
Surgical Treatment
The bone is lengthened by surgically applying an external fixation device to the leg. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins, or both. A small crack is made in the bone and the frame creates tension when the patient or family member turns its dial. This is done several times each day. The lengthening process begins approximately five to 10 days after surgery. The bone may lengthen 1 millimeter per day, or approximately 1 inch per month. Lengthening may be slower in a bone that was previously injured. It may also be slower if the leg was operated on before. Bones in patients with potential blood vessel abnormalities, such as cigarette smokers, may also need to be lengthened more slowly. The external fixator is worn until the bone is strong enough to support the patient safely. This usually takes about three months for each inch. Factors such as age, health, smoking and participation in rehabilitation can affect the amount of time needed.
Mortons Neuroma Remedy
Overview
 Put simply - Morton's neuroma is a swollen (inflamed) nerve in the ball of the foot, commonly between the base of the second and third toes. Patients experience numbness and pain in the affected area, which is relieved by removing footwear and/or massaging the foot. A neuroma is a tumor that arises in nerve cells, a benign growth of nerve tissue that can develop in various parts of the body. In Morton's neuroma the tissue around one of the nerves leading to the toes thickens, causing a sharp, burning pain in the ball of the foot. A sharp severe pain, often described as a red hot needle may come on suddenly while walking. There may also be numbness, burning and stinging in the toes. Although it is labeled a neuroma, many say it is not a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).
Put simply - Morton's neuroma is a swollen (inflamed) nerve in the ball of the foot, commonly between the base of the second and third toes. Patients experience numbness and pain in the affected area, which is relieved by removing footwear and/or massaging the foot. A neuroma is a tumor that arises in nerve cells, a benign growth of nerve tissue that can develop in various parts of the body. In Morton's neuroma the tissue around one of the nerves leading to the toes thickens, causing a sharp, burning pain in the ball of the foot. A sharp severe pain, often described as a red hot needle may come on suddenly while walking. There may also be numbness, burning and stinging in the toes. Although it is labeled a neuroma, many say it is not a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).
Causes
The exact cause of Morton's neuroma is not known. However, it is thought to develop as a result of long-standing (chronic) stress and irritation of a plantar digital nerve. There are a number of things that are thought to contribute to this. Some thickening (fibrosis) and swelling may then develop around a part of the nerve. This can look like a neuroma and can lead to compression of the nerve. Sometimes, other problems can contribute to the compression of the nerve. These include the growth of a fatty lump (called a lipoma) and also the formation of a fluid-filled sac that can form around a joint (a bursa). Also, inflammation in the joints in the foot next to one of the digital nerves can sometimes cause irritation of the nerve and lead to the symptoms of Morton's neuroma.
Symptoms
Feelings of numbness, tingling or tenderness in the ball of the foot (the area just behind the base of the toes) are some of the first signs of a condition known as Morton?s Neuroma. However, the condition is somewhat unpredictable, and symptoms may vary from patient to patient. Generally, however, the discomfort gets worse rather than better, and the patient may feel pain or a burning sensation that radiates out to the toes. Eventually, wearing shoes becomes uncomfortable (or even unbearable), and the patient may complain that the feeling is similar to that of having a stone bruise, or walking on a marble or pebble constantly, even though no there is no trauma to the skin, and no visible bump or lump on the sole of the foot.
Diagnosis
An MRI scan (magnetic resonance imaging) is used to ensure that the compression is not caused by a tumor in the foot. An MRI also determines the size of the neuroma and whether the syndrome should be treated conservatively or aggressively. If surgery is indicated, the podiatrist can determine how much of the nerve must be resected. This is important, because different surgical techniques can be used, depending on the size and the position of the neuroma. Because MRIs are expensive, some insurance companies are reluctant to pay for them. If the podiatrist believes an MRI is necessary, he or she can persuade the insurance company to pay for it by presenting data to support the recommendation.
Non Surgical Treatment
Treaments may include wearing wider shoes to reduce the squeezing force on the foot. Adding a specially made padding to shoes to offload the pressure on the ball of the foot (called a metatarsal dome) Addressing the foot and lower limb biomechanics. This involves looking at foot stability and if needed prescribing an orthotic device to correct your foot position. Anesthetic & Cortisone injections. This is done when the above treatments are insufficient. The trauma is sometimes so great that conservative treatment cannot control the inflammation or cause of the pain. A series of injections are performed to control the inflammation or to temporarily settle the nerve. An ultrasound and cortisone injection can be prescribed by your podiatrist.
Surgical Treatment
Surgery to remove the neuroma may be recommended if more conservative treatment does not solve the problem. While surgery usually relieves or completely removes the symptoms, it often leaves a permanent numb feeling at the site of the neuroma.
Prevention
While Morton?s Neuroma has been an ongoing topic of clinical investigation, the condition is in some cases difficult to either treat or prevent. Experimental efforts involving the injection of muscle or bone with chemicals such as alcohol, as well as suturing, and covering affected areas with silicone caps have been attempted, with varying success.
 Put simply - Morton's neuroma is a swollen (inflamed) nerve in the ball of the foot, commonly between the base of the second and third toes. Patients experience numbness and pain in the affected area, which is relieved by removing footwear and/or massaging the foot. A neuroma is a tumor that arises in nerve cells, a benign growth of nerve tissue that can develop in various parts of the body. In Morton's neuroma the tissue around one of the nerves leading to the toes thickens, causing a sharp, burning pain in the ball of the foot. A sharp severe pain, often described as a red hot needle may come on suddenly while walking. There may also be numbness, burning and stinging in the toes. Although it is labeled a neuroma, many say it is not a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).
Put simply - Morton's neuroma is a swollen (inflamed) nerve in the ball of the foot, commonly between the base of the second and third toes. Patients experience numbness and pain in the affected area, which is relieved by removing footwear and/or massaging the foot. A neuroma is a tumor that arises in nerve cells, a benign growth of nerve tissue that can develop in various parts of the body. In Morton's neuroma the tissue around one of the nerves leading to the toes thickens, causing a sharp, burning pain in the ball of the foot. A sharp severe pain, often described as a red hot needle may come on suddenly while walking. There may also be numbness, burning and stinging in the toes. Although it is labeled a neuroma, many say it is not a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).Causes
The exact cause of Morton's neuroma is not known. However, it is thought to develop as a result of long-standing (chronic) stress and irritation of a plantar digital nerve. There are a number of things that are thought to contribute to this. Some thickening (fibrosis) and swelling may then develop around a part of the nerve. This can look like a neuroma and can lead to compression of the nerve. Sometimes, other problems can contribute to the compression of the nerve. These include the growth of a fatty lump (called a lipoma) and also the formation of a fluid-filled sac that can form around a joint (a bursa). Also, inflammation in the joints in the foot next to one of the digital nerves can sometimes cause irritation of the nerve and lead to the symptoms of Morton's neuroma.
Symptoms
Feelings of numbness, tingling or tenderness in the ball of the foot (the area just behind the base of the toes) are some of the first signs of a condition known as Morton?s Neuroma. However, the condition is somewhat unpredictable, and symptoms may vary from patient to patient. Generally, however, the discomfort gets worse rather than better, and the patient may feel pain or a burning sensation that radiates out to the toes. Eventually, wearing shoes becomes uncomfortable (or even unbearable), and the patient may complain that the feeling is similar to that of having a stone bruise, or walking on a marble or pebble constantly, even though no there is no trauma to the skin, and no visible bump or lump on the sole of the foot.
Diagnosis
An MRI scan (magnetic resonance imaging) is used to ensure that the compression is not caused by a tumor in the foot. An MRI also determines the size of the neuroma and whether the syndrome should be treated conservatively or aggressively. If surgery is indicated, the podiatrist can determine how much of the nerve must be resected. This is important, because different surgical techniques can be used, depending on the size and the position of the neuroma. Because MRIs are expensive, some insurance companies are reluctant to pay for them. If the podiatrist believes an MRI is necessary, he or she can persuade the insurance company to pay for it by presenting data to support the recommendation.
Non Surgical Treatment
Treaments may include wearing wider shoes to reduce the squeezing force on the foot. Adding a specially made padding to shoes to offload the pressure on the ball of the foot (called a metatarsal dome) Addressing the foot and lower limb biomechanics. This involves looking at foot stability and if needed prescribing an orthotic device to correct your foot position. Anesthetic & Cortisone injections. This is done when the above treatments are insufficient. The trauma is sometimes so great that conservative treatment cannot control the inflammation or cause of the pain. A series of injections are performed to control the inflammation or to temporarily settle the nerve. An ultrasound and cortisone injection can be prescribed by your podiatrist.

Surgical Treatment
Surgery to remove the neuroma may be recommended if more conservative treatment does not solve the problem. While surgery usually relieves or completely removes the symptoms, it often leaves a permanent numb feeling at the site of the neuroma.
Prevention
While Morton?s Neuroma has been an ongoing topic of clinical investigation, the condition is in some cases difficult to either treat or prevent. Experimental efforts involving the injection of muscle or bone with chemicals such as alcohol, as well as suturing, and covering affected areas with silicone caps have been attempted, with varying success.
Treating Leg Length Difference With Shoe Lifts
There are two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is anatomically shorter than the other. Through developmental phases of aging, the brain senses the gait pattern and identifies some variation. The body usually adapts by tilting one shoulder to the "short" side. A difference of less than a quarter inch isn't grossly excessive, doesn't need Shoe Lifts to compensate and ordinarily won't have a profound effect over a lifetime.

Leg length inequality goes largely undiscovered on a daily basis, however this condition is simply corrected, and can eradicate quite a few cases of lumbar pain.
Treatment for leg length inequality usually consists of Shoe Lifts . These are affordable, frequently costing under twenty dollars, in comparison to a custom orthotic of $200 or higher. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most common condition affecting people today. Over 80 million men and women experience back pain at some stage in their life. It is a problem that costs businesses huge amounts of money every year on account of lost time and output. New and superior treatment solutions are constantly sought after in the hope of decreasing the economic influence this issue causes.

People from all corners of the earth suffer the pain of foot ache due to leg length discrepancy. In these types of situations Shoe Lifts can be of worthwhile. The lifts are capable of decreasing any pain and discomfort in the feet. Shoe Lifts are recommended by numerous expert orthopaedic practitioners".
In order to support the human body in a balanced manner, the feet have a vital role to play. Inspite of that, it is sometimes the most neglected region of the human body. Many people have flat-feet meaning there may be unequal force placed on the feet. This will cause other areas of the body like knees, ankles and backs to be affected too. Shoe Lifts ensure that correct posture and balance are restored.

Leg length inequality goes largely undiscovered on a daily basis, however this condition is simply corrected, and can eradicate quite a few cases of lumbar pain.
Treatment for leg length inequality usually consists of Shoe Lifts . These are affordable, frequently costing under twenty dollars, in comparison to a custom orthotic of $200 or higher. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most common condition affecting people today. Over 80 million men and women experience back pain at some stage in their life. It is a problem that costs businesses huge amounts of money every year on account of lost time and output. New and superior treatment solutions are constantly sought after in the hope of decreasing the economic influence this issue causes.

People from all corners of the earth suffer the pain of foot ache due to leg length discrepancy. In these types of situations Shoe Lifts can be of worthwhile. The lifts are capable of decreasing any pain and discomfort in the feet. Shoe Lifts are recommended by numerous expert orthopaedic practitioners".
In order to support the human body in a balanced manner, the feet have a vital role to play. Inspite of that, it is sometimes the most neglected region of the human body. Many people have flat-feet meaning there may be unequal force placed on the feet. This will cause other areas of the body like knees, ankles and backs to be affected too. Shoe Lifts ensure that correct posture and balance are restored.
Diagnosing Calcaneal Spur

Overview
A heel spur is a bony projection on the sole (bottom) of the heel bone. This condition may accompany or result from severe cases of inflammation to the structure called plantar fascia. The plantar fascia is a fibrous band of connective tissue on the sole of the foot, extending from the heel to the toes. Heel spurs are a common foot problem resulting from excess bone growth on the heel bone. The bone growth is usually located on the underside of the heel bone, and may extend forward toward the toes. A painful tear in the plantar fascia between the toes and heel can produce a heel spur and/or inflammation of the plantar fascia. Because this condition is often correlated to a decrease in the arch of the foot, it is more prevalent after the ages of six to eight years, when the arch is fully developed.
Causes
When a bone is subjected to pressure, rubbing, or other stress over long periods, it tries to repair itself by building extra bone. This extra bone is what is referred to as a ?spur?. Many form as part of the aging process when cartilage breaks down in the joints.

Symptoms
Pain and discomfort associated with heel spurs does not occur from the spur itself. The bone growth itself has no feeling. However, as you move, this growth digs into sensitive nerves and tissue along the heel of the foot, resulting in severe pain. Pain can also be generated when pushing off with the toes while walking. Swelling along the heel is also common.
Diagnosis
Most patients who are suffering with heel spurs can see them with an X-ray scan. They are normally hooked and extend into the heel. Some people who have heel spur may not even have noticeable symptoms, although could still be able to see a spur in an X-ray scan.
Non Surgical Treatment
The majority of heel spurs are treated with non-surgical interventions. These can relieve pain, but may take from about 3 months to up to a year for symptoms to resolve. Rest, icing, and over-the-counter anti-inflammatory or prescription medications can help ease symptoms. Cortisone injections may also be used. Physical therapists may instruct you to perform stretching exercises to help relax the tissues in the heel. Your doctor may recommend custom orthotics or shoe inserts to position and cushion your heel. Night splints can help position the heel and arch of the foot while you sleep. Some doctors may recommend extracorporeal shock wave therapy (ESWT). This treatment uses energy pulses to start the repair process in the heel tissues. ESWT is recommend when other non-surgical treatments have failed.
Surgical Treatment
Have surgery if no other treatments work. Before performing surgery, doctors usually give home treatments and improved footwear about a year to work. When nothing else eases the pain, here's what you need to know about surgical options. Instep plantar fasciotomy. Doctors remove part of the plantar fascia to ease pressure on the nerves in your foot. Endoscopy. This surgery performs the same function as an instep plantar fasciotomy but uses smaller incisions so that you'll heal faster. However, endoscopy has a higher rate of nerve damage, so consider this before you opt for this option. Be prepared to wear a below-the-knee walking cast to ease the pain of surgery and to speed the healing process. These casts, or "boots," usually work better than crutches to speed up your recovery time.
Best Ways To Spot Heel Spur

Overview
A heel spur is caused by the displacement of calcium on the bone that forms on the underside of the heel, it may be one small bony protrusion or a collection of tiny, irregularly shaped growths on the bone of the heel, which is called the calcaneum. Heel spurs are sometimes painful, described as a knife digging into the heel and other times, a heel spur goes unnoticed and is only detected by an X-ray.
Causes
Heel spurs develop as an abnormal growth in the heel bone due to calcium deposits that form when the plantar fascia pulls away from the heel. This stretching of the plantar fascia is usually the result of over-pronation (flat feet), but people with unusually high arches (pes cavus) can also develop heel spurs. Women have a significantly higher incidence of heel spurs due to the types of footwear often worn on a regular basis.

Symptoms
You may or may not experience any symptoms with your heel spurs. It is normally the irritation and inflammation felt in the tissues around your heel spur that cause discomfort. Heel pain is one of the first things you may notice, especially when pushing off the ball of your foot (stretches the plantar fascia). The pain can get worse over time and tends to be stronger in the morning, subsiding throughout the day; although it does return with increased activity. A sharp, poking pain in your heel that feels like you're stepping on a stone can often be felt while standing or walking. You will sometimes be able to feel a bump on the bottom of your heel, and occasionally bruising may appear.
Diagnosis
A heel spur is often seen on X-ray as a bony protrusion, which can vary in size. However, because a Heel Spur only indicates increased load on the plantar fascia, and not pain, an ultra sound may be required to assess other actual cause of the heel pain such and may include checking to see if the plantar fascia is inflamed or degenerated.
Non Surgical Treatment
Podiatric Care for heel spur syndrome may involve keeping the fascia stretched out by performing exercises. Your doctor may also suggest for you to be seen by a physical therapist. You probably will be advised on the best shoes to wear or some inserts for your shoes. Your podiatrist may suggest that a custom made orthotic be made to allow your foot to function in the most ideal way especially if you have excessive pronation. A heel lift may be used if you have a leg length discrepancy. Medical treatment may include anti-inflammatory oral medications or an injection of medication and local anesthetic to reduce the swelling and decrease pain. If a bursitis is present the medication may greatly improve the symptoms. Your podiatric physician may also recommend a surgical procedure to actually fix the structural problem of your foot.
Surgical Treatment
Surgery involves releasing a part of the plantar fascia from its insertion in the heel bone, as well as removing the spur. Many times during the procedure, pinched nerves (neuromas), adding to the pain, are found and removed. Often, an inflamed sac of fluid call an accessory or adventitious bursa is found under the heel spur, and it is removed as well. Postoperative recovery is usually a slipper cast and minimal weight bearing for a period of 3-4 weeks. On some occasions, a removable short-leg walking boot is used or a below knee cast applied.
Prevention
If you have not yet developed this condition, you can take steps to protect yourself from it. Most importantly, make it a rule to wear properly fitted footwear. Avoid shoes that have become worn down in the heel, and don't choose shoes that cause you to walk in an abnormal fashion. Maintaining a healthy weight will ensure that undue pressure isn't being put on the ligaments, tendons and bones of your feet. If your job requires a great deal of time on your feet, or if you exercise regularly, be sure to balance periods of activity with periods of rest for your feet.